Coronavirus
AnalysisThink COVID is becoming like the flu? Here’s how much worse it still is
The Cupertino Courier January 19, 2022
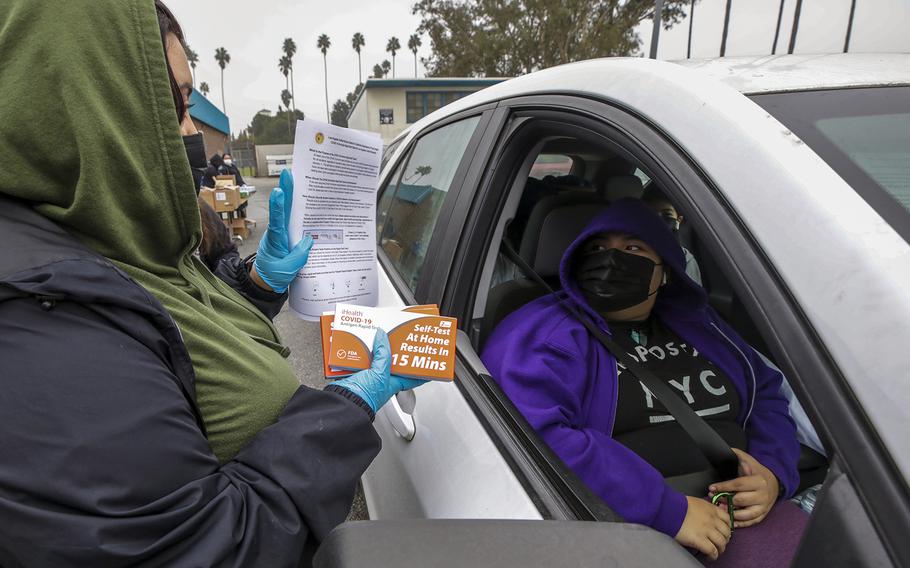
Wendy Lopez gives in-home COVID test kits provided by Los Angeles Unified School District free at Johnnie L. Cochran Jr. Middle School on Friday, Jan. 7, 2022, in Los Angeles, California. (Irfan Khan, Los Angeles Times/TNS)
Stars and Stripes is making stories on the coronavirus pandemic available free of charge. See more stories here. Sign up for our daily coronavirus newsletter here. Please support our journalism with a subscription.
(Tribune News Service) — Bill Gates, the billionaire Microsoft founder and philanthropist who warned that the globe wasn't ready for a pandemic, shared a new prediction last week on the fate of COVID-19: "Once omicron goes through a country, then the rest of the year should see far fewer cases, so COVID can be treated more like seasonal flu."
Right now, that's hard to imagine.
With the U.S. recording more than 750,000 new cases and nearly 2,000 deaths a day from the super-contagious omicron variant, and hospitals in many parts of the country still bracing for the worst, it's difficult to foresee the day we can liken COVID to influenza.
"We've learned to kind of accommodate and live with influenza," said Warner Greene, a virologist at the Gladstone Institutes in San Francisco. "Hopefully we can get there with COVID, but we're not there yet."
There is just no comparison.
A closer look at the numbers two years into the pandemic shows two unmistakable takeaways: COVID killed more than eight times as many Americans in 2021 as the flu killed in the 2017-18 season, the worst in more than a decade. And since the SARS-CoV-2 virus swept the globe, influenza deaths in the U.S. have plummeted by more than 90% as humanity hunkered down.
Studies indicate omicron causes milder illness than earlier COVID variants, but experts and early data again say there is little question: "Omicron is more deadly than the flu," said John Swartzberg, clinical professor emeritus of infectious diseases and vaccinology at UC Berkeley.
"End of story," agreed UCSF infectious disease expert George Rutherford.
For example, even though it's still too early to get a complete picture of the death toll from the ongoing omicron surge, a look at the final week of December 2021, as the holiday spike exploded, is telling.
More than 5,000 people across the U.S. died of COVID the last week of 2021. That's more than three times the number of people — 1,626 — who succumbed to influenza during the deadliest week of the alarming 2017-18 flu season. And since the coronavirus arrived in 2020, there have been just two weeks in the more than 100 weeks of the pandemic when fewer than 1,600 people died from COVID.
Another startling comparison: About 52,000 people died during that 2017-18 flu season. During typical influenza years, the virus claims roughly half that many lives. But at its peak last January, the coronavirus claimed more than 25,000 lives in the U.S. in one week — on par with the death total for an entire average flu season.
How about hospitalizations? Influenza is no match for COVID, which is straining our medical system in ways unseen before.
According to Centers for Disease Control and Prevention (CDC) estimates, as many as 41 million people get sick with the flu in a bad season. In 2017-18, about 710,000 people were hospitalized for influenza. In 2021, the U.S. recorded roughly 35 million COVID cases — and more than 2.5 million hospitalizations.
During the pandemic, flu deaths have tanked. Some of the precipitous drop likely has to do with changes brought on by the pandemic. While California and especially other parts of the country are not locked down and sheltering in place like in March 2020, more people are wearing masks in crowded places, working remotely and holding off on travel and indoor dining. The more infectious COVID has thrived despite those measures — but the flu, not so much.
"I think everybody is being much more cautious than prior to COVID," Swartzberg said. "I think that's playing a major role."
Schools, especially in California, are also requiring masking and have been in and out of remote learning — disrupting the classroom environments where flu typically spreads, Rutherford said.
There's also the possibility, Swartzberg said, that "tragically COVID has already culled out the people who are most likely to die of influenza."
Still, traces of a rebound in flu deaths are starting to emerge — although they're difficult to visualize on a scale with COVID because the number of deaths is so vastly different. In December, monthly flu deaths in the U.S. topped 200 for the first time since the pandemic began.
"We may see the numbers here go up" this season, Swartzberg said.
Weekly U.S. flu deaths — which went from the triple digits into the double digits when the pandemic hit and have stayed there, sometimes dipping into the single digits — are likely to rebound in the coming years, Swartzberg thinks, which means the health care system will need to adapt.
Exactly when that happens remains to be seen and could depend in part on future coronavirus variants.
"Let me consult my crystal ball," joked Rutherford.
In the future, Swartzberg said, medical interventions such as vaccines, monoclonal antibodies and antiviral treatments could finally deliver us to a point where COVID could end up being a fair comparison to the flu. Moderna has said it even hopes to have a combined available in 2023. But, he said, "it's going to be a process."
(c)2022 The Cupertino Courier (San Jose, Calif.)
Visit The Cupertino Courier (San Jose, Calif.) at www.mercurynews.com/cupertino
Distributed by Tribune Content Agency, LLC.