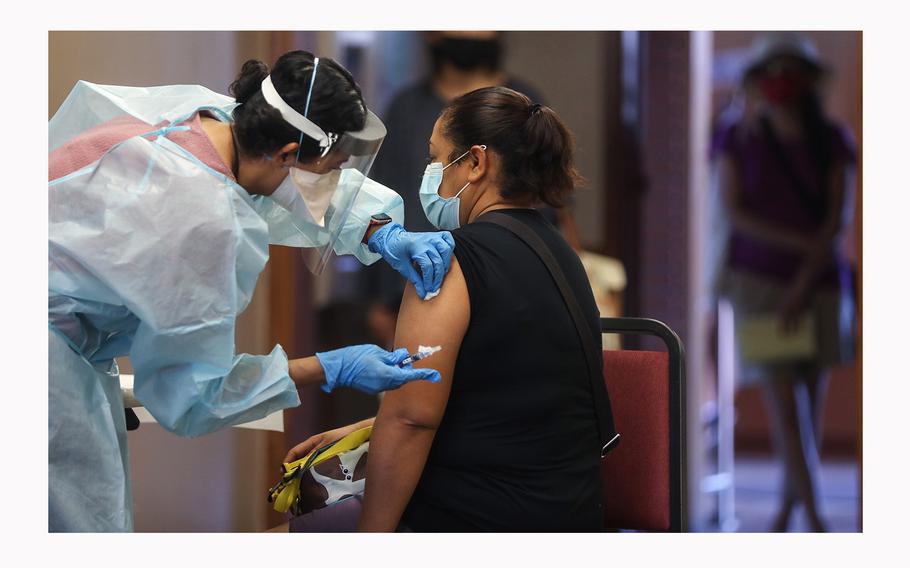
A nurse prepares to administer a flu vaccination shot to a woman at a free clinic held at a local library on Oct. 14, 2020, in Lakewood, California. (Mario Tama/Getty Images/TNS)
(Tribune News Service) — So far, respiratory virus activity in San Diego County has been much more bearable than it was this time last year.
Local labs and medical providers reported 942 coronavirus, 425 flu and 297 respiratory syncytial virus cases to the public health department last week. Last year, the numbers were eye-poppingly higher: 3,441 coronavirus, 2,386 flu, 401 RSV, during the same week.
It’s the same pattern for flu-like symptoms reported by patients visiting local emergency departments. Last week, 4 percent had fevers, coughs and or sore throats compared to 10 percent one year ago.
This is what normal looks like, says Dr. Robert Schooley, infectious disease specialist at UC San Diego. Generally, the heaviest months of activity for respiratory viruses are in the winter. Last year’s early arrival had a lot to do with the years that came before.
“We had a couple of years of artificial suppression with everybody wearing masks (and limiting contact) for COVID, and that allowed the overall population immunity to the other respiratory viruses to decline a bit,” Schooley said. “That’s why we saw them pick up a little earlier and get going in the fall.
“Now we’ve seen a couple rounds with a more normal fraction of the population getting infected, so I think we’re moving back toward a more-traditional pattern.”
None of these threats are static, and the novel coronavirus that causes COVID-19 has continued to mutate even as it causes less severe illness. The latest wastewater analysis from SEARCH, a coalition of local research labs, indicates that a new variant of the virus called BA.2.86 made up 5 percent of circulating virus in San Diego’s largest wastewater district as of Nov. 13.
BA.2.86 has been said to be as big an evolutionary leap as the difference between the original Omicron variant and Delta, it’s predecessor. Does its arrival mean that we are in for a particularly rough winter on the COVID front?
Scripps Research immunologist Kristian Andersen, whose work has delved deep into the complexities of the COVID pandemic in recent years, said in an email Wednesday that while it seems clear that 2.86 will become dominant and cause a steady rise in cases, they will most likely not be severe.
Why would that be the case, given the broad set of new mutations that 2.86 carries?
As Andersen sees it, our immune systems are simply better prepared to respond.
“Our immunity landscape (due to vaccinations and infections) is now so complex that it’s very difficult for the virus to completely break through our immunity wall, and that’s exactly what we’re seeing with BA.2.86,” Andersen said. “The jump it took in evolutionary space is comparable to the one the original Omicron variant took; however, the effect on cases isn’t anywhere near that.
“(It’s) very likely this is simply due to the fact that we keep making our immunity landscape broader, more robust, more complex.”
Environment also plays a significant role in the arrival of runny nose season.
It has been a relatively warm fall thus far, and comfortable outdoor temperatures are known to tamp down the spread of infectious diseases that spread through the air. While many attribute this phenomenon to the fact that people are not crowded together indoors as much as they would be if it were cold and blustery outside, Schooley noted that this is only part of the explanation.
Viruses don’t travel naked through the air, but are generally floating inside the water droplets that spray from a person’s nose and mouth when they cough, sneeze or even talk.
“These tiny packets of water we call aerosols dry out when the humidity is low, and that decreases the particle size which allows them to stay suspended in the air for a longer time,” Schooley said.
That explanation might seem counter-intuitive, especially in San Diego where the winter brings rain and, generally, higher humidity than has recently been experienced, especially when Santa Ana winds dried the air to levels that left everyone itching.
But cold weather, Schooley noted, gets people turning on their furnaces when they’re indoors.
“Most of the heating systems we use put out dry air, and that can cause those aerosol particle sizes to get small really quickly, and that smaller size allows them to float around for longer after somebody breathes or sneezes,” he said.
Will this end up being a severe flu season? It certainly could, and Schooley said that vaccination remains the key to staying out of the emergency room for those who are at the highest risk.
“I think everybody who has any respiratory risk factors or who is older should certainly get all three vaccines, RSV, influenza and COVID,” Schooley said. “In the case of influenza, we know that vaccination decreases a little bit the likelihood of getting infected, but it decreases a lot the likelihood of being severely ill.
“As for COVID, there’s more and more evidence that the more immunity you have, the less likely you are to develop long COVID and the less likely you are to turn up in the hospital with acute COVID.”
©2023 The San Diego Union-Tribune.
Visit sandiegouniontribune.com
Distributed by Tribune Content Agency, LLC.